Bloodborne Pathogens
Bloodborne Pathogens Definition
Bloodborne pathogens, or BBP, are pathogenic microorganisms that are present either in human blood or in other potentially infectious materials (OPIM), and which can cause disease in humans, according to Cal/OSHA CCR Title 8 Section 5193. These pathogens include, but are not limited to, hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV).
Other Potentially Infectious Materials
OPIM is a broad category that, according to Cal/OSHA CCR Title 8 Section 5193, includes the following materials:
- Semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, amniotic fluid, saliva in dental procedures, and all body fluids in situations where you are unable to differentiate between body fluids.
- Any unfixed tissue or organ that is not intact skin, from any human, both living or dead.
-
Any of the following when they are likely or known to contain or be infected
with HBV, HCV, or HIV:
- Any human's or experimental animal's cells, tissue, or organ cultures.
- Any experimental animal's blood or organs
- Any culture medium or solutions.
The following materials are only considered OPIM if blood is visibly present alongside the material:
- Feces
- Saliva
- Sweat
- Tears
- Urine
- Vomit
Bloodborne Pathogens Program Requirements
Universal Precautions
- Wear impervious gloves. Latex, neoprene or other impervious materials are acceptable. Leather gloves do not offer protection from infectious agents. Wash gloves with soap and water or disinfectant before removing.
- Use disinfectants (bleach or quaternary ammonium) on small spills before handling.
- Wash hands immediately after removing gloves. Use soap and water or disinfectant towelettes.
- Wear an impervious apron or suit if the possibility exists of splashing infectious materials onto exposed skin.
- Wear eye protection if the possibility exists of splashing infectious materials into your eyes.
- Wear a face mask if the possibility exists of splashing infectious materials onto your face.
- Report all possible exposure incidents to your supervisor immediately. Employees who have had exposure to potentially infectious materials may have a confidential consultation with a physician.
- Employees who may be exposed to potentially infectious materials can receive a hepatitis B vaccination. (find out if link at https://chw.calpoly.edu/health/vaccinations is how the employee would get the vaccination, or if there's a separate process) (maybe create separate webpage for vaccination process mentioned on page 10 of https://afd.calpoly.edu/ehs/docs/pathogens.pdf)
Training
All faculty, staff, and student employees who work with human blood or body fluids must complete the EHS Bloodborne Pathogen course on the Cal Poly Learning Hub.
Applicability
The Bloodborne Pathogen program covers all University employees who have occupational exposures with blood or potentially infectious materials during their normal job duties. Exposure determination shall be based upon an employee's reasonable potential for exposure to blood or any other infectious materials that they may contact during their job duties. OSHA requires exposure evaluations based on the potential for job-related tasks leading to exposure. The program at Cal Poly is designed to cover those who are at a higher risk of exposure by establishing high, moderate, or low risk categories.
Bloodborne Pathogens Exposure Control
See the Bloodborne Pathogens document for a more comprehensive look at the Exposure Control Plan.
-
Engineering and Work Practice Controls
- The appropriate safety hood will be used, if applicable, based on the specific type of hazard present.
- Departments shall provide hand-washing facilities that are readily accessible to employees. When facilities are not available, employees shall be provided either with an appropriate antiseptic hand cleanser in conjunction with clean cloth/paper towels or antiseptic towelettes. When antiseptic hand cleansers or towelettes or used, hands shall be washed with soap and running water as soon as feasible.
- Employees shall wash their hands immediately, or as soon as possible, after the removal of gloves or other personal protective equipment.
- No eating, drinking, smoking, or application of cosmetics, lip balm, or handling of contact lenses in work areas where the possibility of exposure exists.
- No foods or drink will be stored or consumed in areas where bloodborne pathogens may be present. This includes storage in refrigerators, freezers, and cabinets, and on shelves and countertops.
- Contaminated needles or sharps will not be recapped, bent, or broken unless the supervisor can demonstrate that no alternative is feasible or that such action is required by a specific medical procedure. Such bending, recapping, or needle removal must be accomplished through the use of a mechanical device or a one-handed technique.
- Immediately, or as soon as possible after use, all potentially contaminated sharps will be placed in a puncture-proof, labelled, and leak-proof container, then disposed of by methods outlined on Cal Poly's Waste Disposal page. The same applies for all potentially infectious protruding objects.
- After use, or as soon as possible after use, reusable sharps will be placed in the appropriate containers for sterilization or reprocessing.
- The lab supervisor or manager is responsible for ensuring that employees and students wear the proper personal protective equipment.
- Mouth pipetting/suctioning of blood or other potentially infectious materials is prohibited.
- All procedures must minimize splashing, spraying, spattering, and generatin of droplets of infectious substances.
-
Personal Protective Equipment (PPE)
Personal protective equipment (PPE) will be made available to employees and students upon entry into laboratory and work areas where infectious materials may be present. This equipment will be removed immediately upon leaving these work areas and placed in the appropriate receptacle for storage, washing, decontamination, or disposal. This equipment includes:
Gloves
- Disposable gloves will be worn when the employee or student has the potential for direct skin contact with infectious materials. Disposable gloves shall be properly disposed of if visibly soiled, torn, or damaged. They will not be washed or disinfected for re-use. Gloves are not to be removed or worn outside the work area. Hypoallergenic gloves shall be provided to personnel who are allergic to the gloves normally provided.
- Non-disposable gloves used in the handling of potentially infectious material must be washed thoroughly with soap and water prior to removing.
- Handwashing must follow removal of all gloves.
Masks/Eye Protection/Face Shields
- This equipment will be worn singularly or in combination as guidelines specify. They will be worn when the potential exists for spattering, spraying, or splashing droplets or aerosols of blood or any other potentially infectious materials may be present. This applies when the employee's or student's eyes, nose, or mouth are potentially exposed to contamination.
Aprons/Gowns/Lab Coats/Disposable Shoe Covers
- The appropriate protective clothing will be worn when the potential for occupational exposure is present. The garments shall be, but not limited to, aprons, gowns, lab coats, clinical jackets, or any similar protective garment that provides an effective barrier against blood or any other infectious materials. Shoes and/or head covers will be worn as needed or as required by protocol.
The guidelines for the use of personal protective equipment are as follows:
- PPE shall be provided where necessary by the department at no cost to the employee.
- Departments shall train and ensure their employees properly use the PPE available.
- The department must clean, launder, and dispose of PPE at no cost to the employee.
- If a garment is penetrated by blood or other potentially infectious material, the garment shall be removed immediately or as soon as feasible.
- All PPE shall be removed prior to leaving the work area.
- When removed, PPE shall be placed in an appropriately designed area or container for storage, washing, decontamination, or disposal.
- Employees or students who fail to utilize PPE, as required, are subject to disciplinary action as deemed appropriate by the department.
-
Housekeeping and Decontamination
Disinfectants and/or germicides shall be applied to working area surfaces to ensure the area is maintained in a clean and sanitary condition. A written policy with a schedule which outlines methods for decontamination and disinfection shall be implemented in these work areas where bloodborne pathogens may be used. All equipment and working surfaces shall be disinfected routinely after use of blood or any other potentially infectious materials.
- Working surfaces and equipment shall be cleaned after completion of working procedures, when these items are overtly contaminated, immediately after a spill of potentially infectious materials, routinely after the end of the work shift, or prior to maintenance or servicing.
- Surfaces where infectious materials are used shall be protected with coverings such as imperviously-backed absorbent paper, plastic wrap, or aluminum foil. These coverings shall be changed at the end of every shift or as necessary.
- Broken glassware which may potentially be contaminated shall be picked up by tongs, forceps, broom, dust pan, etc. At no time will employees pick up potentially contaminated broken glass with their bare hands. Protective clothing, e.g. goggles, face mask, or leather gloves, shall be worn during the cleanup.
- All containers, bins, pails, cans, or similar receptacles intended for use in disposal of these waste will have a lid or top on the container. These containers will be collected on a daily basis or when the container becomes full. The reusable containers will be inspected, cleaned, and disinfected on a routine basis or as soon as possible after visible contamination.
- Reusable items that may be potentially infectious will be decontaminated before washing or reprocessing.
- Laundry that potentially may be contaminated shall be collected from employees and cleaned on a daily basis. The employees who normally generate potentially contaminated garments shall be informed of the location and specific container for the garments. These garments will not be rinsed or sorted at the locatin of their removal. The employees who collect, wear, or process these garments shall wear the proper PPE (gloves, lab coats, etc.) and receive training for handling bloodborne pathogens. The containers these garments are collected in will be labelled as biohazardous and described as soiled laundry. They must be closeable and leak-proof bags or containers and must be color-coded.
-
First Aid and CPR Responders
Cal Poly has a number of employees that are CPR and first aid trained or may be put into a position where they might assist another employee or student with minor injuries involving contact with blood or other infectious materials. While pre-exposure precautions do not apply, precautions must be taken by these individuals to avoid exposure. Cal Poly employees must use the following guidelines to avoid possible exposure:
- All departments should have, as part of their required first aid supplies, several pairs of disposable gloves.
- Serious injuries involving loss of blood should be reported immediately to University Police by dialing 911 on campus phones.
- Contact with the blood of an injured person should be avoided. For non-serious first aid injuries, allow the injured person to treat themself or assist by transporting them to the Health Center. If contact and exposure is unavoidable, wear protective gloves.
- If blood or body fluid exposure occurs, a Report of Employee Injury must be filed with Human Resources. Contact your supervisor, Department Administrator, Safety Coordinator or call Environmental Health and Safety at ext. 6-6662. EH&S must be notified immediately.
- Do not attempt to clean up any of the spilled blood, if present. This is considered biohazardous medical waste and must be cleaned up and disposed of according to waste regulations. Notify work control at ext. 3494.
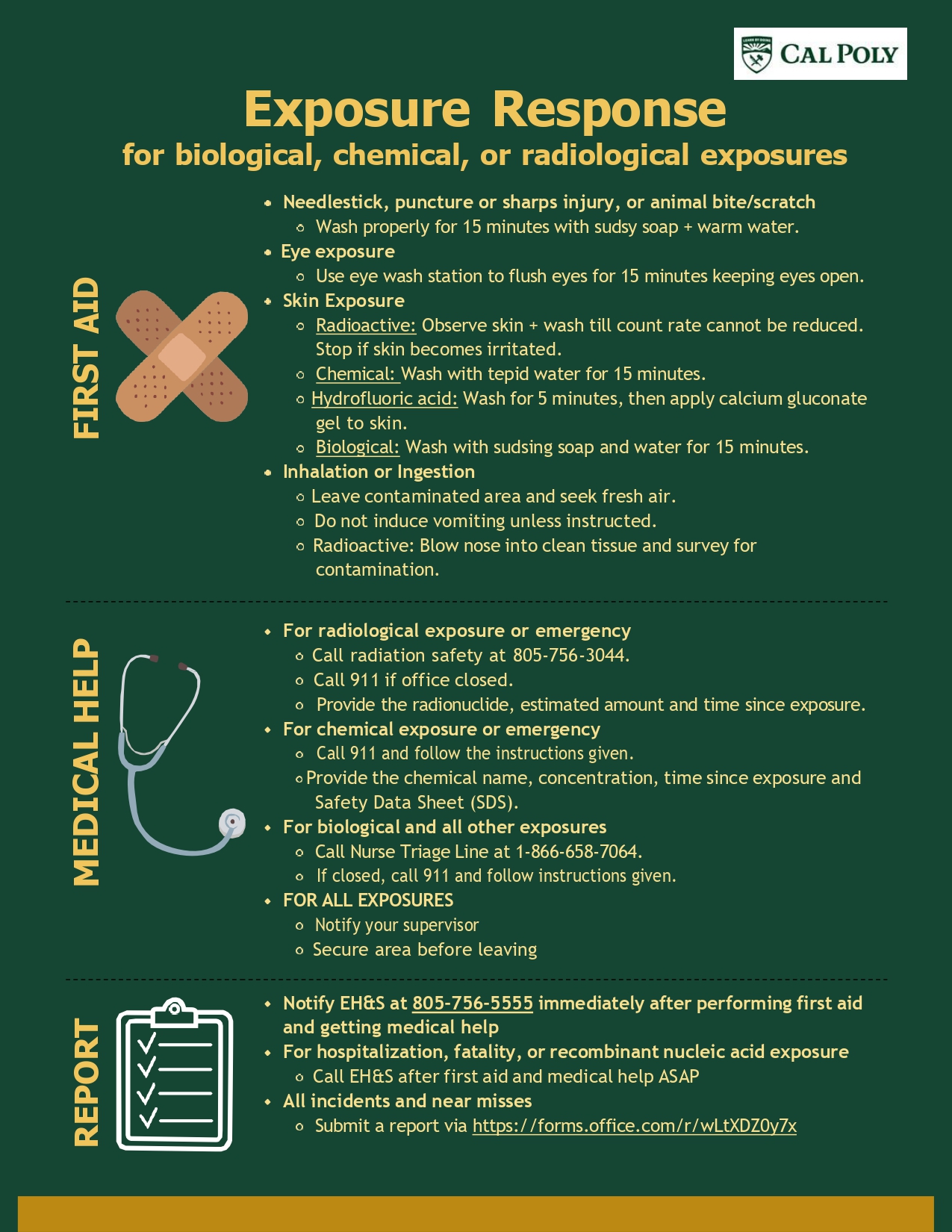
Bloodborne Pathogens Exposure Response
Open the flyer here to copy text or click on links.
Bloodborne Pathogens Exposure Reporting
Reporting an Exposure to Bloodborne Pathogens
- The exposure incident must be reported to the supervisor, Department Administrator or Department Safety Coordinator before the end of the work day in which the exposure occurred.
- A Report of Employee Injury must be filed with Human Resources.
- The supervisor must document the route(s) of exposure using the Exposure Report Form.
See page 8 of the Bloodborne Pathogens document for further details.
Post-Exposure Evaluation and Follow-up
After a report of an exposure incident, the following procedures must be followed:
- A confidential medical evaluation and follow-up must be made available to the exposed employee. Elements of this evaluation include:
- The supervisor will identify and document the source individual, unless they can establish that identification is infeasible or prohibited by state or local law.
- The source individual's blood will be tested ASAP after consent is obtained in order to determine HBV, HCV, and HIV infectivity. If consent is not obtained, the supervisor will establish that legally required consent cannot be obtained.
- When the source individual's consent is not required by law, the source individual's blood, if available, shall be tested and the results documented.
- The source individual's testing results will be made available to the exposed employee, and the employee will be informed that this is confidential information.
- The department will provide for collection and testing of the exposed employee's blood for HBV, HCV, and HIV serological status as follows:
- The exposed employee's blood shall be collected ASAP and tested after consent is obtained.
- If the employee consents to baseline blood collection, but does not give consent at that time for HIV serologic testing, the sample shall be preserved for at least 90 days. If, within 90 days of the exposure incident, the employee elects to have the baseline sample tested, such testing shall be done ASAP.
- Additional testing shall be made available as recommended by the U.S. Public Health Service.
- The employer shall provide for post-exposure prophylaxis, when medically indicated, as recommended by the U.S. Public Health Service.
- The employer shall provide for counseling and evaluation of reported illnesses.
See page 10 of the Cal Poly Bloodborne Pathogen Program and Exposure Control Plan for further details.
